Barriers to Intergenerational Health
While much has been written about the transmission of income and education across generations, “much less is known about how health is passed down between generations," Wang notes, highlighting a gap in the existing research. Emphasizing that health is a crucial factor in determining overall well-being, as it affects everything from mental health to economic productivity and social mobility, she asserts that good health is linked to better educational outcomes, higher earning potential, and improved labor market performance. Poor health, on the other hand, is associated with lower educational attainment, reduced employment prospects, and higher rates of chronic illness.
Wang’s research approach centers on recognizing the multiple challenges in implementing maternal health-oriented policies. Having identified limited access to healthcare services as a significant barrier, she considers how, in many low-income and rural areas, “access to quality healthcare is constrained by poor infrastructure, lack of transportation, and shortages of healthcare professionals, making it difficult for pregnant women to receive essential care.”
Another obstacle is the prohibitive cost of healthcare. In countries where maternal health services are not subsidized or free, the financial burden of out-of-pocket expenses for transportation, medications, and other related costs can prevent women from accessing necessary care. Furthermore, Wang shows that low levels of maternal health education can contribute to poor health-seeking behaviors. “Many women may not recognize the warning signs of complications, may not fully understand the importance of prenatal care, or may be unaware of their rights to healthcare services,” she says.
Measuring Health Outcomes Across Generations
Wang acknowledges the difficulties in studying intergenerational health mobility, as it cannot be neatly defined and measured by observable metrics such as income or education. Health is much more subjective and varies from person to person. To gauge health outcomes, researchers must therefore rely on diverse and sometimes imprecise indicators, such as the presence of chronic diseases.
Moreover, to examine intergenerational mobility, researchers need data that includes health information for both parents and children. Such datasets are not always readily available, and those that do exist often lack the necessary granularity and long-term tracking to provide meaningful insights.
To overcome these challenges, Wang draws on a variety of panel data that tracks individuals over time, as well as survey data and self-reported status. For Wang, longitudinal studies are crucial for understanding how health disparities manifest and evolve over time.
Using data from the Indonesia Family Life Survey, she combines subjective measures like self-reported health and objective measures such as pulse, BMI, hypertension, and anemia to capture a more complete picture of health mobility. This approach expands beyond previous studies, which typically relied on fewer health indicators and focused on developed countries. Her study includes a broad range of health variables and provides a unique look at the role of gender and socioeconomic factors in shaping health outcomes across generations.
Wang uses two primary methods for measuring intergenerational health mobility: one following the Intergenerational Health Association, which regresses children's health outcomes on those of their parents, and rank-rank regressions, which examine the persistence of health outcomes by analyzing percentile ranks. These techniques, adapted from income mobility research, allow her to assess health persistence and mobility across generations.
Future Directions and Policy Impact
Wang’s time at APARC has been instrumental in shaping and refining her research. "The opportunity to engage with experts from various fields [...] opened my eyes to new ways of thinking about my research," she shared. "The collaborative environment at APARC also made me realize how much I can learn from perspectives outside my immediate area of focus.”
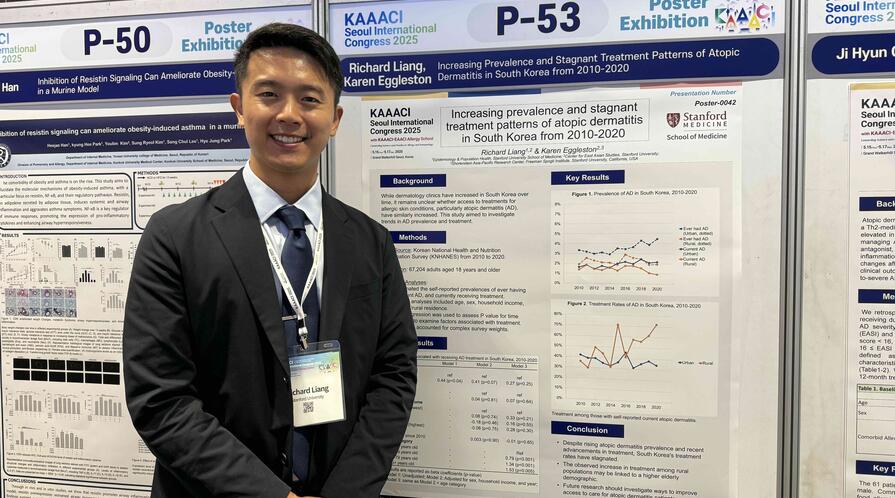
Wang credits Stanford’s vibrant academic environment, with its rich array of seminars and talks, to broadening her understanding of Southeast Asian health systems, a subject she was less familiar with. She expressed gratitude to APARC faculty for their “invaluable guidance for both my research and my life at Stanford.” In particular, APARC’s Asia Health Policy Program Director Karen Eggleston “dedicated a significant amount of time to advising my work, introducing me to key researchers in my field, and sharing the valuable resources that I might benefit from on campus,” Wang said.
Looking ahead, she is excited to continue exploring the role of health in intergenerational mobility, particularly in the Southeast Asian context, and plans to expand her research into the health effects of pollution, an area she has already begun to investigate. Wang also hopes to contribute to policymaking that addresses health inequality. By providing a deeper understanding of how health disparities are perpetuated across generations, she aims to inform policies that could improve health outcomes and reduce inequality in developing countries.
Wang’s research on intergenerational health mobility offers a fresh and much-needed perspective on the crucial yet understudied role of health in social mobility. She hopes her research helps policymakers and scholars address health inequalities that perpetuate socioeconomic disadvantage across generations.